Case Discussions & Teaching Points | January – February 2026
A curated summary of the most educational clinical discussions from the EndoCollab WhatsApp group
CASE 1: Classification and Workup of Gastric Neuroendocrine Tumors
A case of multiple gastric polyps with one confirmed as a Grade 1 NET prompted an excellent discussion on the classification, workup, and surveillance of gastric NETs.
Key Teaching Points
▸ Gastric NETs are classified into three types: Type 1 (80% of cases, associated with autoimmune atrophic gastritis, pernicious anemia, B12 deficiency), Type 2 (associated with Zollinger-Ellison syndrome/hypergastrinemia), and Type 3 (neuroendocrine carcinoma, usually solitary and >1 cm — the most dangerous).
▸ Both Type 1 and Type 2 are associated with hypergastrinemia but via different mechanisms. Type 1 and 2 are usually well-differentiated with low Ki-67 index, multiple, and <1 cm.
▸ A solitary gastric NET is more concerning (Type 3), while multiple lesions suggest Type 1 or 2.
▸ NBI/I-scan/FICE cannot differentiate between Type 1 and Type 2, but advanced imaging endoscopy is useful for identifying additional small NETs that may have been missed on white light.
▸ Differentiation between Type 1 and 2 relies on clinical features, endoscopic appearance, and laboratory tests (gastrin levels, anti-parietal cell antibodies, etc.).
▸ If resected with clear surgical margins and no other NET seen on PET, surveillance endoscopy alone may suffice for Grade 1 NETs.
▸ Other polyps should be biopsied and histopathology reviewed. Colonoscopy should be considered to evaluate for polyposis syndromes.
▸ EUS and DONET assessment should be considered for lymph node staging.
CASE 2: Difficult ERCP Cannulation — The Submucosal Injection Technique
A case of failed biliary cannulation in a patient with choledocholithiasis and a small papillary orifice generated valuable advice on advanced cannulation strategies.

Key Teaching Points
▸ Use a tapered-tip sphincterotome (e.g., Boston Scientific) with a 0.025-inch guidewire for difficult cannulations.
▸ If the guidewire enters the pancreatic duct, consider placing a 5 Fr protective plastic stent (single pigtail, 4–6 cm) and then reattempt biliary cannulation.
▸ The submucosal injection technique (described in a GIE video) can aid cannulation by elevating the papillary tissue. When using this technique, have a fully covered metal stent available in case of perforation — the stent seals the defect.
▸ Needle knife precut sphincterotomy remains an option if the papilla is visible intraduodenally.
▸ Careful assessment of papillary anatomy is critical — the orifice may be located higher than expected.
CASE 3: Botox Injection Technique for Achalasia
A practical discussion on the technical aspects of endoscopic Botox injection for achalasia, particularly useful for endoscopists starting this procedure.
Key Teaching Points
▸ Injection site: 1–1.5 cm above the Z-line, in 4 quadrants.
▸ Dose: 25 units per quadrant, for a total of 100 units.
▸ Calculate and account for the dead space of the injection needle before starting — there will be residual Botox that needs to be flushed out.
▸ Use 1.2 mL of saline to flush the last portion of Botox through the needle catheter.
▸ Prepare a pre-measured syringe of saline flush to ensure dosing accuracy.
▸ There is no reliable endoscopic method to confirm muscularis propria injection depth — clinical response serves as the primary endpoint.
▸ Consistent symptomatic improvement is expected in experienced hands, particularly in elderly patients who are not candidates for more definitive therapy.
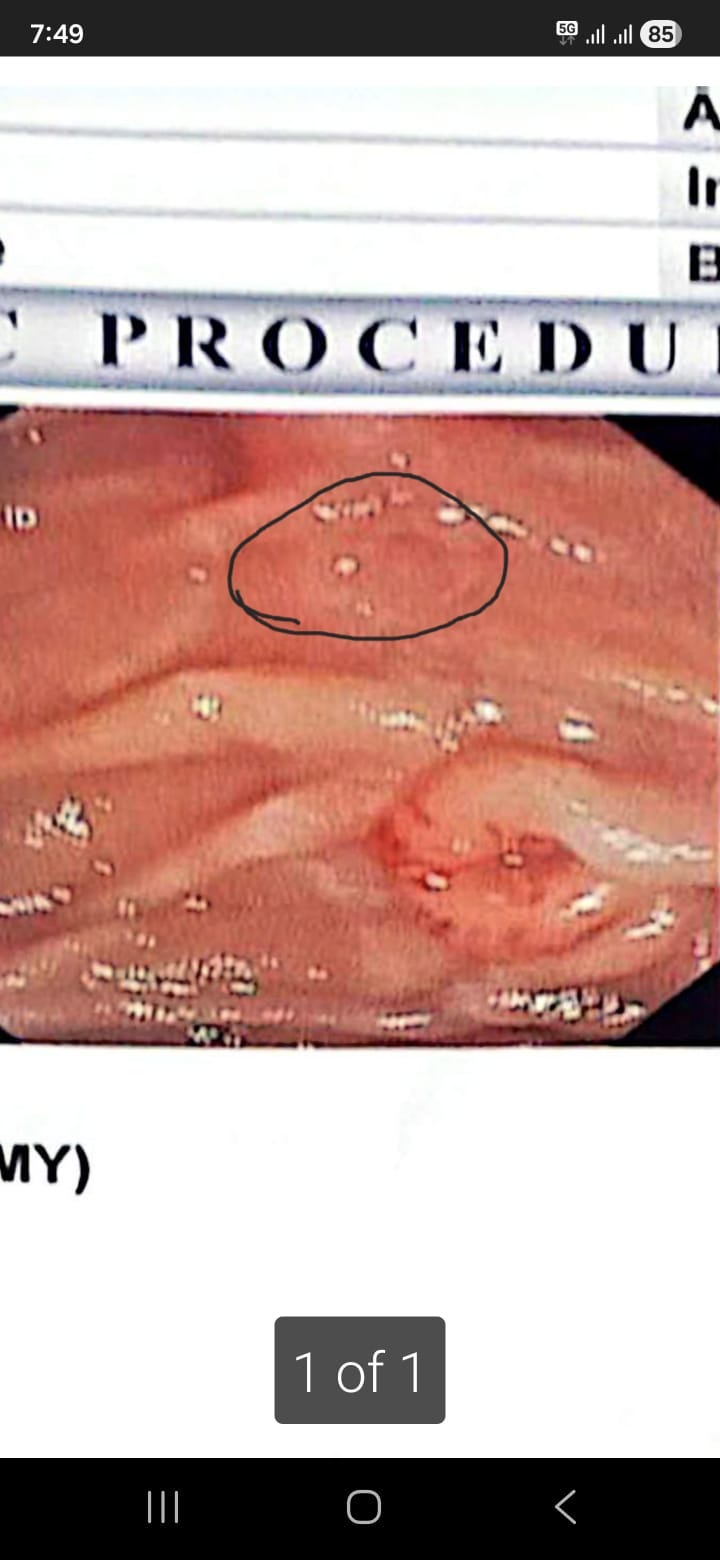
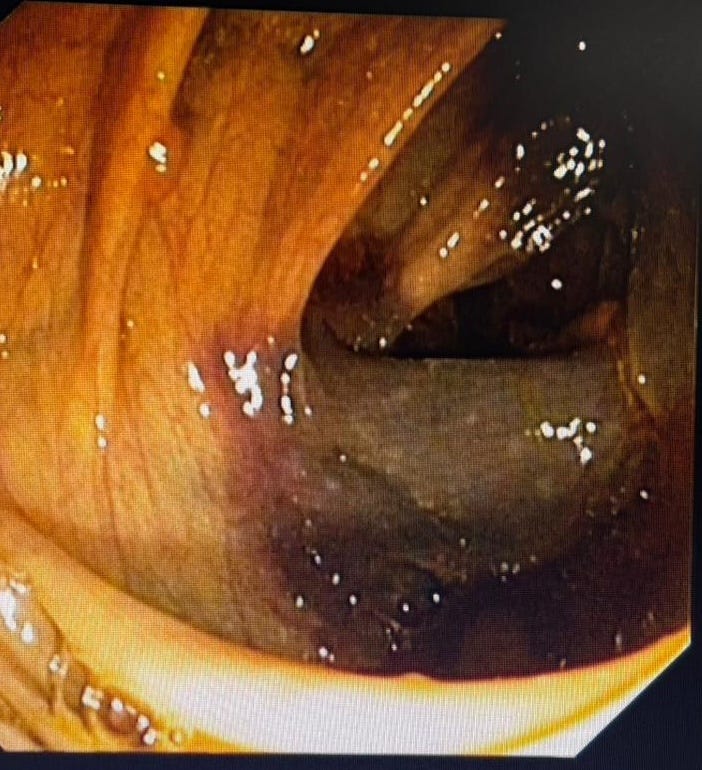
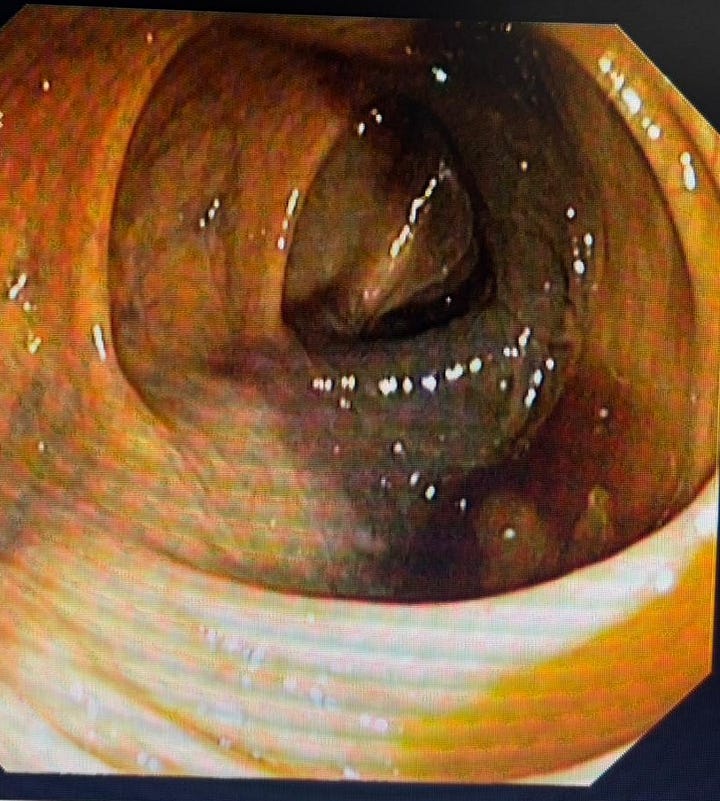
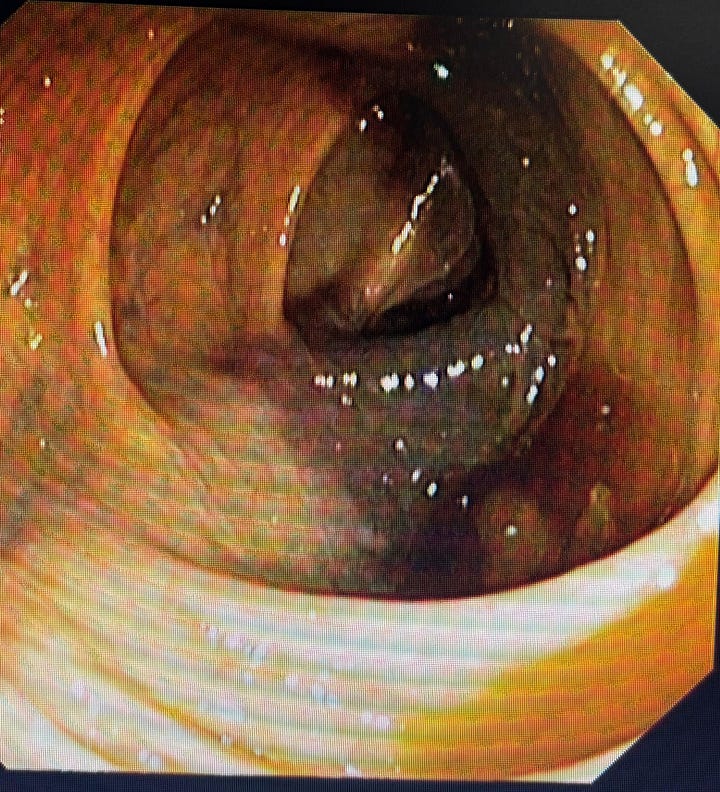
CASE 4: Hemorrhagic Ascending Colon — Ischemic Colitis on Anticoagulation
A 68-year-old female post aortic valve replacement on DOACs presented with per-rectal bleeding and anemia with INR >7. Colonoscopy revealed hemorrhagic ascending colon mucosa.

Key Teaching Points
▸ Endoscopic appearance is consistent with ischemic colitis or intramural hematoma in the setting of supratherapeutic anticoagulation.
▸ CT angiography is recommended to assess for vascular compromise, especially given the risk of transmural necrosis and perforation in subsequent days.
▸ Antibiotics are reasonable given the risk of bacterial translocation in ischemic colitis — necrosis can be transmural.
▸ In the absence of active bleeding with stabilized hemoglobin, expectant management with repeat colonoscopy after INR normalization is acceptable.
▸ Restarting DOACs requires careful multidisciplinary consideration — balance the risk of recurrent ischemia versus thromboembolic events.
▸ Emergency right hemicolectomy carries high morbidity in elderly patients and should be a last resort.
▸ CT angiography should be the first step to guide the urgency of any intervention.
You have seen 3 cases. There are 21 more — and they are the ones your colleagues are bookmarking.
What is behind the paywall:
The exact gold probe settings and coaptive technique that prevent rebleeding (and the duodenal mistake that taught one colleague the hard way)
The stenting protocol after sphincteroplasty that protects against perforation
Duodenal lesions in cirrhosis that look like adenomas but could bleed catastrophically if biopsied
A named syndrome that explains elevated lipase with no pancreatitis — and four other diagnoses most of us overlook
The fish bone rule that prevents fatal complications in delayed presentations
Mid-esophageal varices too wide for EVL: the full management algorithm from an active case discussion
Plus cases on EoE step-down therapy, ERCP in tracheostomy patients, juvenile polyp technique, scope trauma recognition, and more
Every case distilled into clear teaching points with image references. Real discussions. Real expertise. Real cases.
Upgrade now and read the full issue.


