Common Types of Pancreatic Cysts and Their Characteristics
A practical overview for endoscopists navigating the complex landscape of pancreatic cystic lesions
Understanding Pancreatic Cysts: A Clinical Guide to the Six Most Common Types
A practical overview for endoscopists navigating the complex landscape of pancreatic cystic lesions
When you encounter a pancreatic cyst during endoscopy or cross-sectional imaging, the differential diagnosis can feel overwhelming. However, understanding the six most common types—and their distinct characteristics—provides a solid foundation for clinical decision-making.
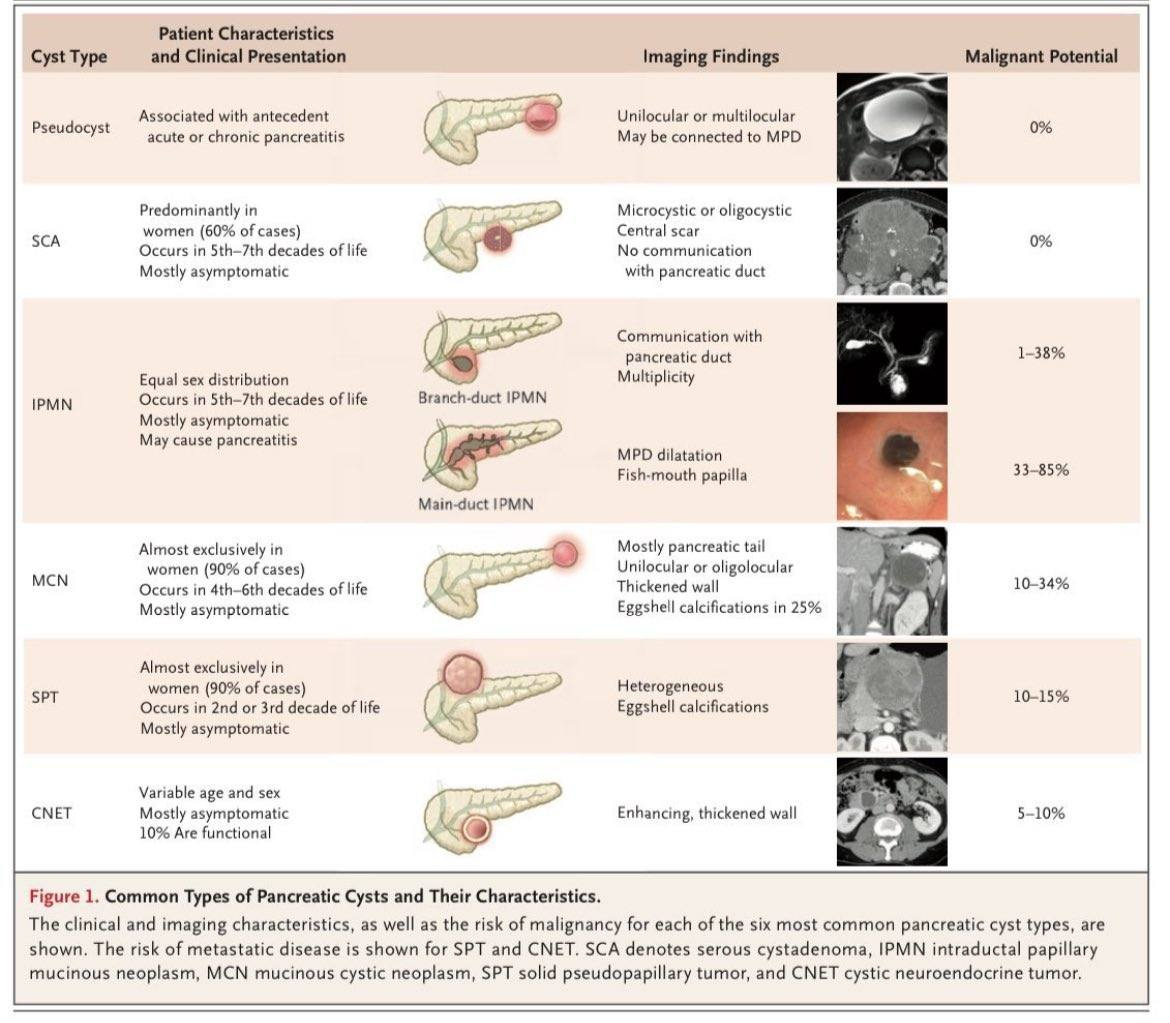
The figure above presents a comprehensive overview that we reference frequently in practice. Let me walk you through what makes each type unique based on the clinical and imaging characteristics shown.
The Benign Spectrum: Pseudocysts and Serous Cystadenomas
Pseudocysts carry 0% malignant potential and are associated with antecedent acute or chronic pancreatitis. The imaging shows these lesions as unilocular or multilocular and may be connected to the main pancreatic duct (MPD).
Serous cystadenomas (SCAs) also demonstrate 0% malignant potential. These lesions predominantly occur in women (60% of cases) and present in the 5th-7th decades of life. Most patients remain asymptomatic. The characteristic imaging appearance shows microcystic or oligocystic lesions with a central scar and no communication with the pancreatic duct.
The Variable Risk Category: IPMNs
Intraductal papillary mucinous neoplasms (IPMNs) show equal sex distribution and occur in the 5th-7th decades of life. Most patients are asymptomatic, though these lesions may cause pancreatitis.
Branch-duct IPMNs demonstrate communication with the pancreatic duct and show multiplicity on imaging. Their malignant potential ranges from 1-38%.
Main-duct IPMNs cause MPD dilatation and display the characteristic "fish-mouth papilla" appearance. These lesions carry a significantly higher malignant potential of 33-85%.
The Female-Predominant Lesions: MCNs and SPTs
Mucinous cystic neoplasms (MCNs) occur almost exclusively in women (90% of cases) and present in the 4th-6th decades of life. Most patients remain asymptomatic. These lesions typically appear in the pancreatic tail as unilocular or oligolocular masses with thickened walls. Eggshell calcifications occur in 25% of cases. The malignant potential is 10-34%.
Solid pseudopapillary tumors (SPTs) also show overwhelming female predominance (90% of cases) but present earlier, in the 2nd or 3rd decades of life. Most patients are asymptomatic. The imaging shows heterogeneous lesions with eggshell calcifications. These carry a 10-15% malignant potential.
The Variable Entity: Cystic Neuroendocrine Tumors
Cystic neuroendocrine tumors (CNETs) demonstrate variable age and sex distribution. Most patients remain asymptomatic, and 10% of these lesions are functional. The imaging appearance shows enhancing, thickened walls. The malignant potential is 5-10%.
Key Clinical Insights
This systematic approach to pancreatic cysts provides a framework for clinical decision-making based on:
Patient demographics: Age and sex patterns vary significantly between lesion types
Clinical presentation: Most pancreatic cysts are asymptomatic regardless of type
Imaging characteristics: Ductal communication, location, and cyst appearance provide crucial diagnostic clues
Malignant potential: Ranges from 0% for benign lesions to up to 85% for main-duct IPMNs
Understanding these fundamental patterns serves as the foundation for appropriate patient care and evidence-based management decisions.
What's your experience with these pancreatic cyst subtypes? Have you found particular imaging characteristics or patient factors that help guide your diagnostic approach? Share your thoughts in the comments below.
Struggling with Complex Pancreatic Cyst Cases?
You're not alone. Every endoscopist faces cases where that "simple cyst" on imaging turns out to be far more complex, and you need expert guidance to navigate the malignant potential spectrum.
That's exactly why we created:
📚 NEW: The EndoCollab Guide for GI Bleeding → The first GI Atlas based on real-life scenarios, novel endoscopic tips and tricks, where ALL GI FELLOWS from a US University teaching hospital contributed ✅ A must-have book 👍🏻
🎯 EndoCollab Membership → Direct access to experts who've differentiated hundreds of pancreatic lesions, plus our searchable library of 1000+ strategies
Because when you're looking at a main-duct IPMN with an 85% malignant potential, you need proven diagnostic approaches, not guesswork.

