EndoCollab WhatsApp Chat Summary: December 2025
8 Challenging Cases, 425+ Expert Insights: Your December Learning Digest
Welcome to the latest edition of the EndoCollab Newsletter! This issue covers the key discussions and learning points from our group over the past month. We’ve seen a wide array of interesting cases, from challenging polypectomies to rare syndromes and important clinical pearls. This summary aims to capture the essence of these discussions for our ongoing education and reference.
Case 1: The Appendiceal Orifice Polyp - A Technical Challenge
Case Summary: A 44-year-old male was found to have a 10-12mm polyp at the appendiceal orifice, sparking a lively debate on the best resection technique.
Key Teaching Points:
•The Challenge of Location: Polyps at the appendiceal orifice present a unique technical challenge due to the difficult angle and the risk of involving the appendix itself.
•EMR with a Cap: Several members recommended EMR with a distal cap to stabilize the position and ensure a controlled and complete resection.
•EFTR - A Double-Edged Sword: Endoscopic Full-Thickness Resection (EFTR) was discussed as an option, but with the significant caveat that it carries a risk of iatrogenic appendicitis.
•Surgical Option: A laparoscopic appendiceal wedge resection was also proposed as a legitimate and safe option, offering a clear histological statement on margins.
•Underwater EMR: The discussion also highlighted underwater EMR as a viable technique.
•Favorable Morphology: The lesion was a Granular LST 0IIa, which carries a very low risk of submucosal invasion (around 0.9%), making less invasive approaches more favorable.
Case 2: A Large LST in the Right Colon - ESD vs. UEMR
Case Summary: A 40mm Laterally Spreading Tumor (LST) of mixed type (IIa+IIs) with a JNET 2B classification in the right colon of a multimorbid patient led to a discussion on the optimal resection strategy.
Key Teaching Points:
•ESD as the Gold Standard: For a lesion with these characteristics (large size, JNET 2B), ESD is generally the recommended technique to achieve an en bloc resection.
•FTRD as an Alternative: Full-Thickness Resection Device (FTRD) was also mentioned as a potential alternative.
•Pragmatic Approach: In this case, due to the patient’s comorbidities and the lesion’s position, the endoscopist opted for underwater EMR, which was successful in achieving a complete resection. This highlights the importance of tailoring the approach to the individual patient and clinical context.
You’re Reading the Recap. But the Real Learning Happened Live.
These eight cases sparked 425 messages in our WhatsApp group during December alone. While you’re reading the summary now, EndoCollab members were in the discussion as it happened—asking questions, sharing their approaches, and debating techniques in real-time.
The difference? Members learn by participating, not just reading. When one of our members faced a similar appendiceal polyp two days after this discussion, they knew exactly what to do because they’d been part of the conversation.
→ Join the Discussion as a Founding Member - Get immediate access to our expert WhatsApp group where cases like these unfold live, plus unlock all premium courses and case libraries.
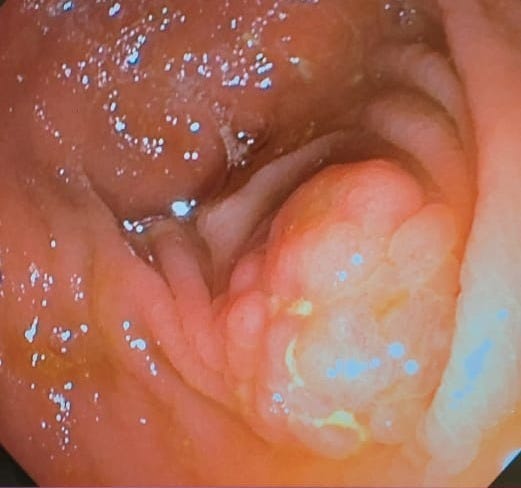
Case 3: A Rare Finding - Blue Rubber Bleb Nevus Syndrome
Case Summary: A series of images showcased the characteristic lesions of Blue Rubber Bleb Nevus Syndrome, a rare vascular disorder.
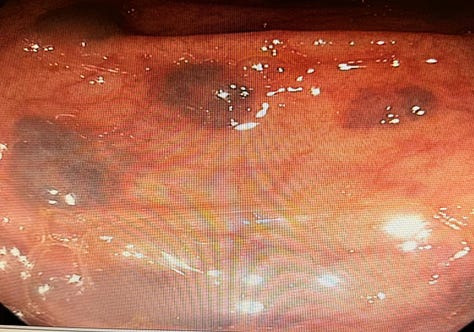
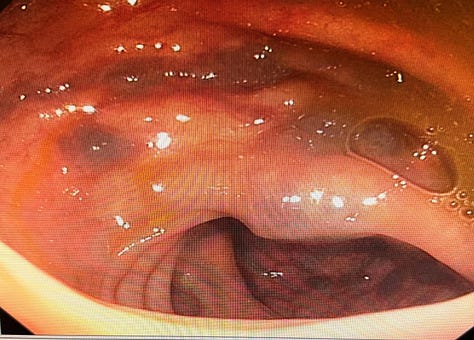
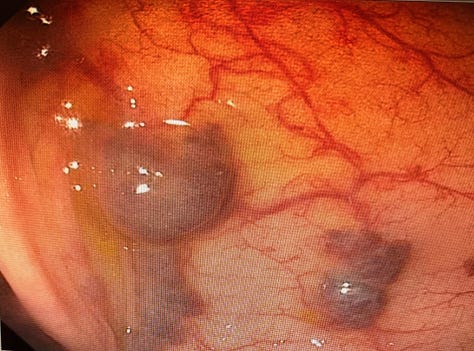
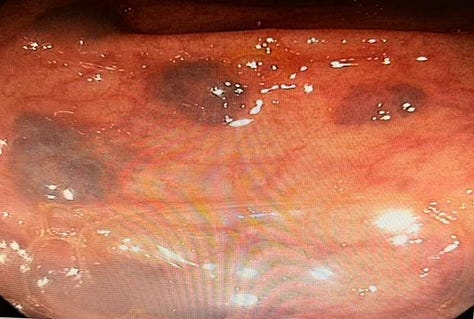
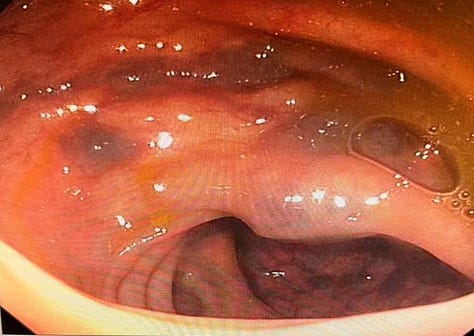
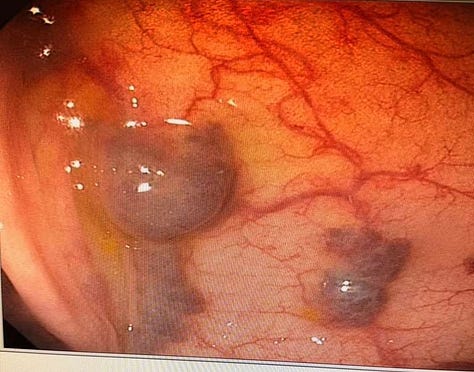
Key Teaching Points:
•Recognizing the Syndrome: This case served as a great reminder of the endoscopic appearance of this rare syndrome, which is characterized by multiple blue or purple vascular nevi throughout the GI tract and skin.
•Clinical Significance: These lesions can be a source of chronic gastrointestinal bleeding and anemia.
Case 4: The Incidental Esophageal Submucosal Lesion
Case Summary: A small (<1cm) submucosal lesion in the esophagus of a patient with long-term reflux symptoms prompted a discussion on the appropriate workup.
Key Teaching Points:
•EUS for Characterization: The consensus was that EUS is the next best step to characterize the lesion, which was suspected to be a benign leiomyoma.
•No Link to Reflux: The group agreed that the lesion was unlikely to be related to the patient’s reflux symptoms.
•Comprehensive Reflux Workup: For the reflux symptoms, a more comprehensive workup, including pH metry with impedance and motility studies, was recommended.
⚡ Quick Question: How many of these cases have you encountered in your own practice?
If you’re nodding along, thinking “I had a case like this last week,” imagine being able to ask our 1,600+ member community for real-time input. In December alone, members posted 8 challenging cases and received expert feedback within minutes—not days.
Upgrade to Founding Member and join today’s discussion. The last case was posted 3 hours ago.
Case 5: A Puzzling Duodenum - Ischemia vs. Inflammation
Case Summary: Images of a duodenum with white-topped folds sparked a differential diagnosis discussion.
Key Teaching Points:
•Ischemia as a Possibility: The white tops of the folds raised suspicion for ischemia, a less common but important consideration.
•Inflammatory Differentials: Other possibilities discussed included chronic duodenitis with atrophic tissue or lymphangiectasia.
•Biopsy is Key: The discussion underscored that biopsy is essential to differentiate between these possibilities and make a definitive diagnosis.
Case 6: Severe Esophagitis - A Broad Differential
Case Summary: An 82-year-old diabetic and hypertensive woman presented with odynophagia and was found to have severe esophagitis, leading to a wide-ranging differential diagnosis discussion.
Key Teaching Points:
• Comprehensive Differential: The group considered a broad differential, including:
• Boerhaave syndrome
• Severe GERD (Grade D)
• Drug-induced esophagitis (bisphosphonates, doxycycline, KCL)
• Infectious causes (CMV, HSV, Candida)
• Ischemia (Acute Esophageal Necrosis)
• Eosinophilic Esophagitis
• Vasculitis (Pemphigus, IgA)
• Acute Esophageal Necrosis: This rare entity, also known as “black esophagus,” was discussed as a possibility, especially in elderly patients with comorbidities. It typically affects the distal third of the esophagus.
• Diagnostic Workup: The recommended workup included a CT chest to rule out perforation, a thorough review of the patient’s drug history, and biopsies to rule out infectious or inflammatory causes.
• Initial Management: High-dose PPI (40mg BD) with a plan for a repeat EGD after healing was the recommended initial management.
Case 7: Pancreatic Rest or Gastric Diverticulum?
Case Summary: An image from a 10-year-old with persistent indigestion showed a lesion that sparked a debate: was it a pancreatic rest or a small gastric diverticulum?
Key Teaching Points:
•A Common Dilemma: This case highlighted a common diagnostic challenge, with opinions in the group split between the two possibilities.
•Endoscopic Features: Pancreatic rests often have a central umbilication, while diverticula are typically smooth outpouchings. However, the appearance can be variable, making a definitive diagnosis on imaging alone difficult.
Case 8: A Rare but Important Complication - Post-Colonoscopy Ischemia
Case Summary: A 60-year-old male smoker developed unilateral acute lower limb ischemia after a colonoscopy, a rare but important complication to be aware of.
Key Teaching Points:
•Mechanism of Injury: The ischemia was thought to be due to dehydration or hypotension from anesthesia in a patient with pre-existing vascular disease.
•Clinical Awareness: This case serves as a crucial reminder to be vigilant for this rare complication, especially in high-risk patients.
Here’s What You Missed in December...
While you’re reading this summary, EndoCollab members are exchanging 425 messages in real time, discussing these cases and many more. They asked follow-up questions. Shared their own similar cases. Learned from experts as the discussions unfolded.
You’re getting the highlight reel. They got the full experience.
Founding Member Benefits:
Immediate WhatsApp access to our expert gastroenterology group (worth $497/year alone)
All premium video courses on advanced endoscopy techniques
Complete case library with 500+ annotated procedures
→ Become a Founding Member
P.S. Next month’s cases are already rolling in—we’ve had 3 complex procedures posted this week. You can read about them in February’s summary—or you can be part of the conversation as it happens. Join the WhatsApp group now.
P.P.S. The appendiceal orifice case from December 2nd? It generated 30+ messages with insights from endoscopists across 4 continents—all within 6 hours. That’s the power of real-time collaboration.