Iron Deficiency - Evaluation and Treatment
Iron Deficiency: What You Need to Know About Testing and Treatment
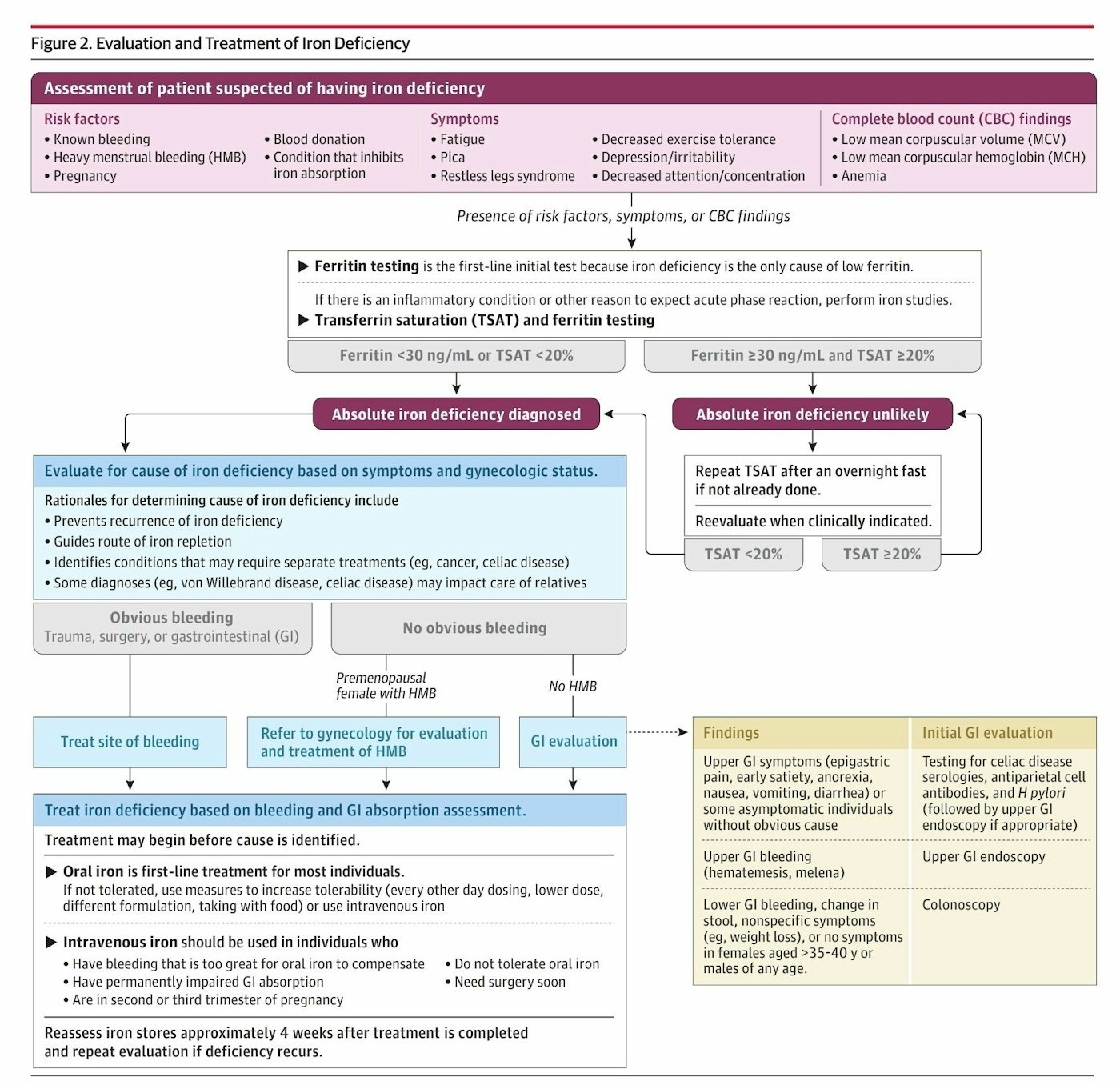
Iron deficiency is more common than you might think, especially among women, blood donors, and those with chronic bleeding. A new comprehensive review in JAMA breaks down the latest approach to diagnosis and treatment.
🚩 Red Flags to Watch For
Risk Factors:
Heavy menstrual bleeding
Known bleeding conditions
Pregnancy
Blood donation
Conditions affecting iron absorption
Symptoms:
Persistent fatigue
Pica (craving ice, starch, etc.)
Restless legs syndrome
Decreased exercise tolerance
Depression/irritability
Poor concentration
🩸 The Testing Strategy
First-line test: Ferritin levels
Ferritin <30 ng/mL OR transferrin saturation (TSAT) <20% = likely iron deficiency
Ferritin ≥30 ng/mL AND TSAT ≥20% = iron deficiency unlikely
Pro tip: If there's inflammation or infection, ferritin can be falsely elevated, so additional iron studies may be needed.
💊 Treatment Essentials
Oral iron is first-line for most people:
Try different formulations or every-other-day dosing if not tolerated
Take with food if causing stomach upset
IV iron is reserved for:
Severe bleeding that oral iron can't keep up with
Poor GI absorption
Can't tolerate oral iron
Need surgery soon
Follow-up: Recheck iron levels about 4 weeks after completing treatment.
🔍 Finding the Root Cause
Once iron deficiency is confirmed, it's crucial to identify WHY it's happening:
Obvious bleeding (heavy periods, GI bleeding) → treat the source
No obvious bleeding → may need GI evaluation, especially in postmenopausal women and men
Source: Iron Deficiency in Adults - A Review, JAMA March 2025
Link: https://jamanetwork.com/journals/jama/fullarticle/2832131
The bottom line: Iron deficiency is treatable, but finding and addressing the underlying cause is just as important as replacing the iron itself.