Quick Case: Portal Hypertensive Duodenopathy
Portal hypertensive duodenopathy (PHD) is frequently overlooked during routine endoscopy, yet represents a significant source of GI bleeding in cirrhotic patients—a diagnosis that requires specific visualization techniques like water immersion and NBI to reveal its characteristic "snakeskin" pattern. Free subscribers receive weekly case highlights, while paid members unlock our complete archive, demonstration videos, comment access, video courses, and our founding members' WhatsApp group for real-time clinical discussion. Ready for the deeper dive? Upgrade and join us.
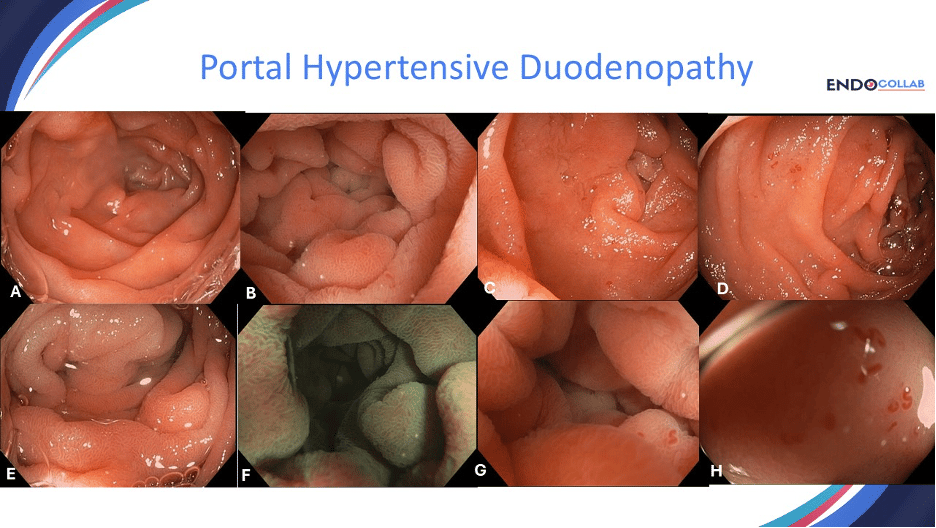
60-year-old male with cirrhosis presented with microcytic anemia and hemoccult positive stools. EGD, colonoscopy and capsule endoscopy were reported as normal. A repeat EGD was performed and portal hypertensive duodenopathy (PHD) was diagnosed both endoscopically and confirmed on histology (Photo)
Portal hypertensive duodenopathy (PHD) is a common condition in patients with cirrhosis and portal hypertension. We have also proposed the name of duodenal antral vascular ectasias (DAVE), as histologically, this condition often mimics GAVE (gastric vascular ectasias).
Importantly, PHD or DAVE is often missed during endoscopy. As you can see from Panel A, which shows a "normal" normal mucosa. However, after using water immersion technique the erythema and edema of the mucosa becomes quite evident. Panel E shows a closer look at the mucosa, with characteristic "snakeskin" pattern. This snakeskin pattern is more evident with NBI (panel F). Patients with PHD or DAVE often have microcytic anemia due to occult or overt gastrointestinal bleeding. Bleeding occurs microscopically from the congested mucosa, but also micro- and macroscopically from tiny angiodysplasias (Panels C, D, G, H). Panel G shows the angiodysplasias using water immersion technique. In Panel H the scope was advanced closer to the mucosa. The angiodysplasias in PHD and DAVE are somewhat different than the classic angiodysplasias occurring in elderly patients or those with Heyde syndrome.
Join the Members-Only Discussion
What visualization techniques have you found most effective for identifying subtle vascular abnormalities like PHD in your cirrhotic patients? Have you encountered cases where standard white-light endoscopy missed PHD that was later revealed with enhanced techniques? We'd love to hear about your diagnostic approach to obscure GI bleeding in portal hypertension and whether you've adopted the water immersion technique in your practice. See you in the comments!