Introduction:
Diagnosing Eosinophilic Esophagitis (EoE) accurately relies heavily on obtaining adequate esophageal biopsies. Despite its distinct characteristics, studies have shown that endoscopic recognition of EoE can be poor.
This guide will cover the essential endoscopic features of EoE to look for, and detail optimal biopsy strategies, including a specific protocol and a practical acquisition trick, to improve your diagnostic yield.
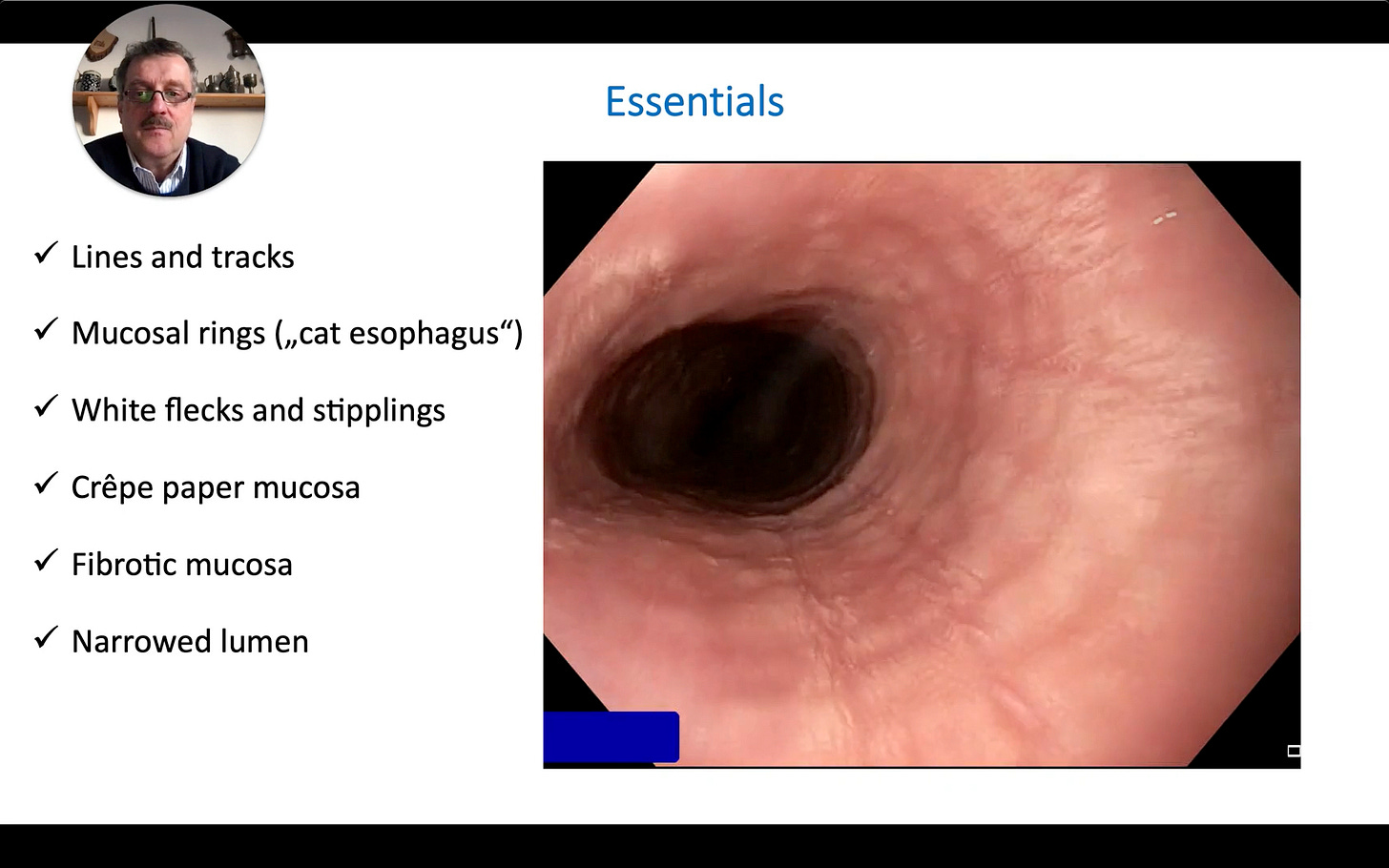
1. Recognizing the Endoscopic Hallmarks of EoE
Before biopsying, it's crucial to identify the endoscopic signs suggestive of EoE. These features can vary but often include:
Lines and Tracks: Longitudinal furrows or linear markings along the esophageal mucosa.
Mucosal Rings (Trachealization or "Cat Esophagus"): Concentric rings giving the esophagus a corrugated or feline appearance.
White Flecks and Stipplings: Small, whitish exudates or spots on the mucosal surface. These can sometimes be confused with candida but are often mixed with other EoE features like lines and tracks. Narrow Band Imaging (NBI) can help appreciate these.
Friable Mucosa (Crepe Paper Mucosa): The esophageal lining may be delicate, easily damaged, or tear with minimal trauma (e.g., scope passage).
Narrowed Lumen and Fibrosis: The esophagus may appear generally narrowed, and the mucosa can exhibit fibrotic changes, feeling stiff or less distensible.
Pay close attention to detail, as these signs guide targeted biopsies.