Why “Close Enough” Isn’t Good Enough in Barrett’s
Barrett’s Esophagus comes in many shapes and sizes. Sometimes it appears as multiple tongues of cylindrical epithelium; other times, it is a single tongue or a completely tubular segment where the esophagus is replaced by columnar-lined epithelium.
Because of this variability, describing findings in a free-text format often leads to confusion. It is essential to have a uniform system to communicate about Barrett’s esophagus so that others can understand our findings and base clinical decisions on accurate data.
The Prague Classification is the gold standard for this communication—it is simple, thorough, and internationally recognized.
This guide breaks down the technique into actionable steps, exactly as demonstrated in the procedure.
Step 1: Evaluate the Hiatal Hernia
Before measuring the Barrett’s segment, you must characterize the environment it lives in. This starts with the hiatal hernia.
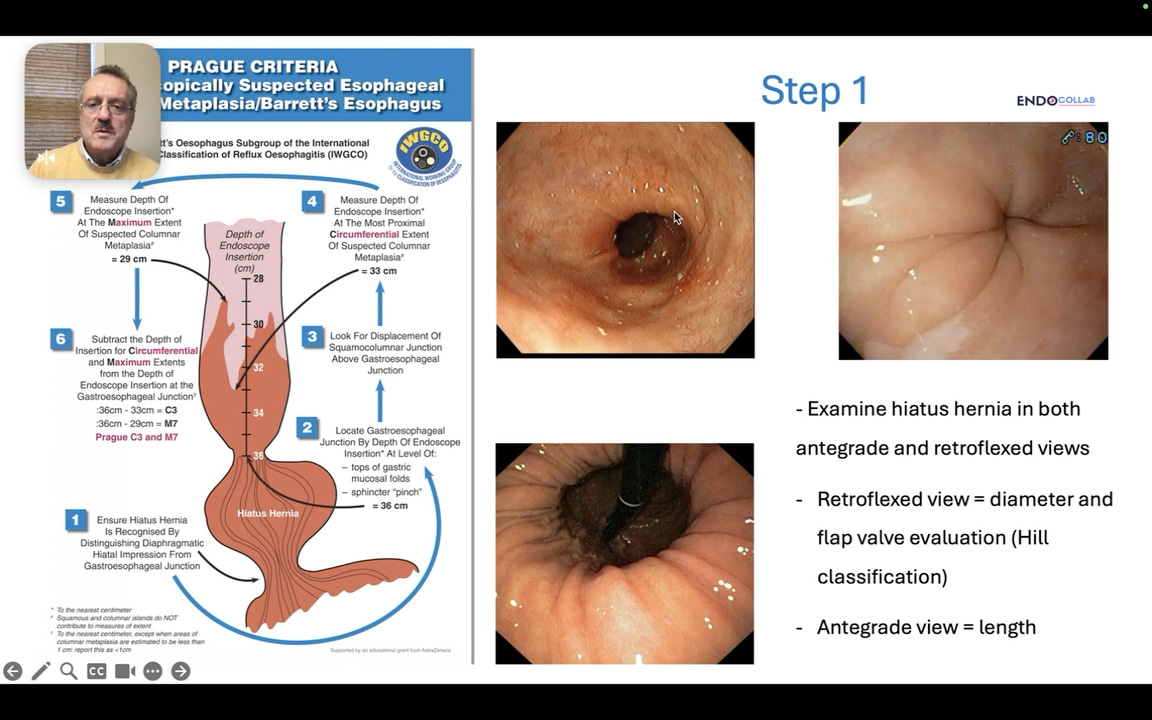
🖥 VISUAL ANALYSIS @ 1:46
The screen displays two endoscopic views side-by-side. On the left, an antegrade view looking down the esophagus into a hernia sac. On the right, a retroflexed view looking up from the stomach, visualizing the hiatus and the flap valve.
Significance: This comparison highlights the importance of using both views to accurately assess the hernia’s length and diameter.
While some experts only perform a retroflexed view to evaluate the diameter and flap valve (Hill classification), it is recommended to use both antegrade and retrograde views.
Antegrade View: As you enter the distal esophagus and pass into the hernia, use the centimeter markings on the endoscope to determine the length of the hernia.
Retroflexed View: Evaluate the diameter or width of the hernia.
The Pitfall of “Pseudo Folds” A common mistake is confusing “pseudo folds” for gastric folds. Usually, the esophagus has no folds; folds begin in the stomach. However, in extensive Barrett’s esophagus, the distal esophagus is dilated and can form folds that mimic a hiatal hernia.
Pro Tip: Look for islands of squamous epithelium. If you see squamous islands on the folds, you are still in the esophagus, not the stomach.
Step 2: Locate the Gastroesophageal Junction (GEJ)
Accurate measurement relies on a fixed starting point: the GEJ.
Method A: Proximal Limit of Gastric Folds The standard method is to identify where the gastric folds end. In a healthy esophagus, this meets the squamous epithelium (the Z-line). In Barrett’s, this junction is replaced by columnar-lined epithelium.
Method B: The Palisade Veins (Kyoto Classification)
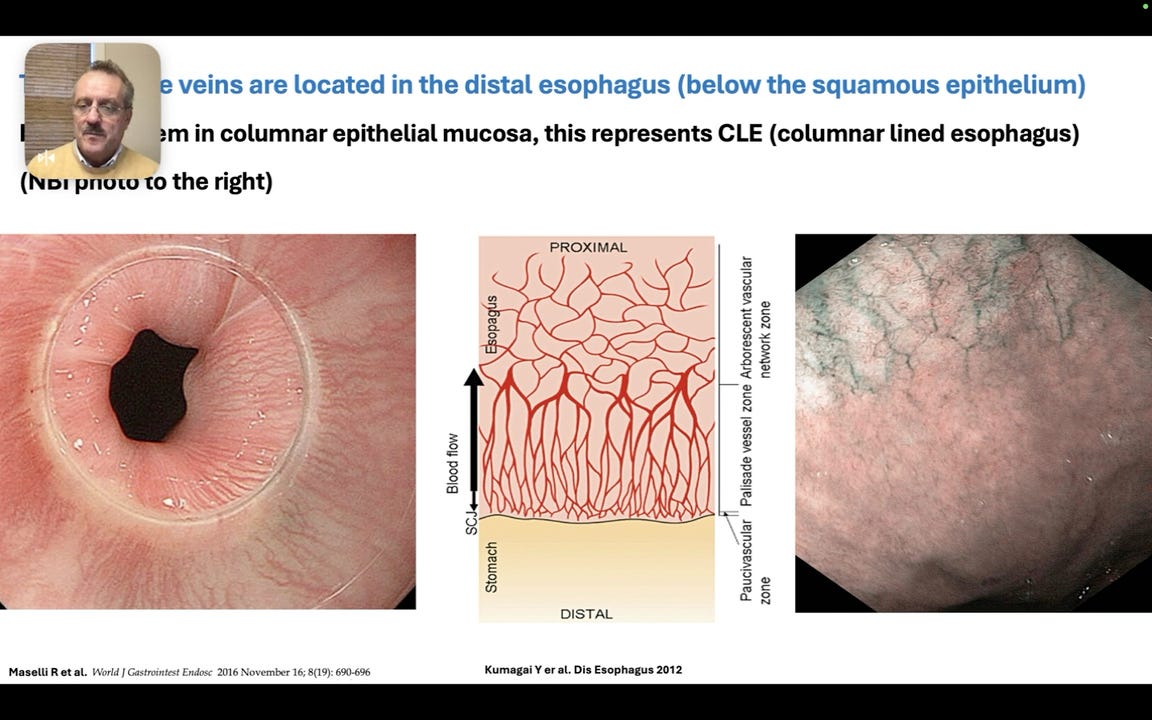
🖥 VISUAL ANALYSIS @ 7:27
The screen shows a high-definition image using Narrow Band Imaging (NBI). Thin, longitudinal vessels are clearly visible running parallel to each other.
Significance: These are palisade veins. They are anatomically located in the distal esophagus and are typically covered by squamous epithelium. In Barrett’s, they become visible through the columnar mucosa.
We recommend using the palisade veins to define the GEJ. If you see palisade veins, you are anatomically in the esophagus, even if the mucosa is columnar.
Step 3: Determine the Extent of Metaplasia
Once the GEJ is fixed, you must assess how far proximal the columnar epithelium extends. You are looking for two specific measurements:
Circumferential Extent (C): The level where the circular coverage of columnar epithelium ends.
Maximal Extent (M): The tip of the longest tongue of columnar epithelium.
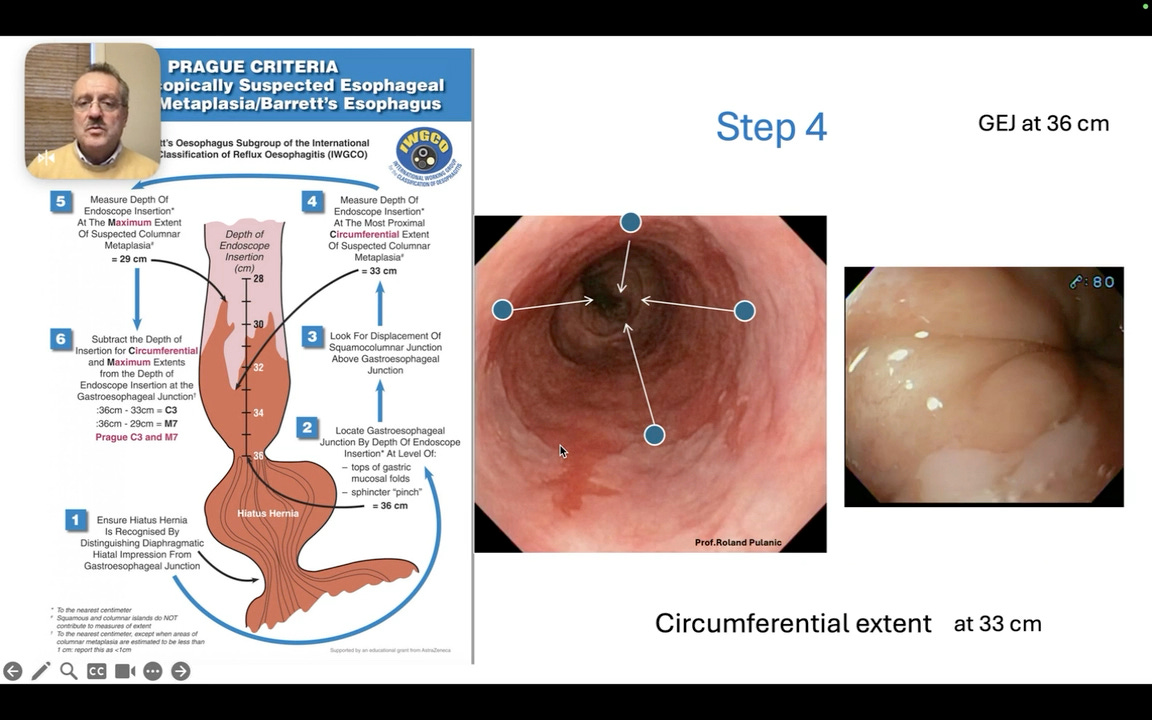
Step 4: Measuring the “C” (Circumferential)
Pull the endoscope back slowly from the GEJ. Stop at the point where the circumferential columnar mucosa ends.
🖥 VISUAL ANALYSIS @ 8:58
The endoscopic view shows a tubular esophagus with reddish columnar mucosa coating the entire circumference. A yellow arrow indicates the precise line where this full-circle coverage stops, transitioning into tongues.
Significance: This is the upper limit for the “C” measurement.
The Calculation:
Locate GEJ (e.g., at 36 cm from incisors).
Locate top of circumferential extent (e.g., at 33 cm).
Subtract the two: 36 - 33 = C3.
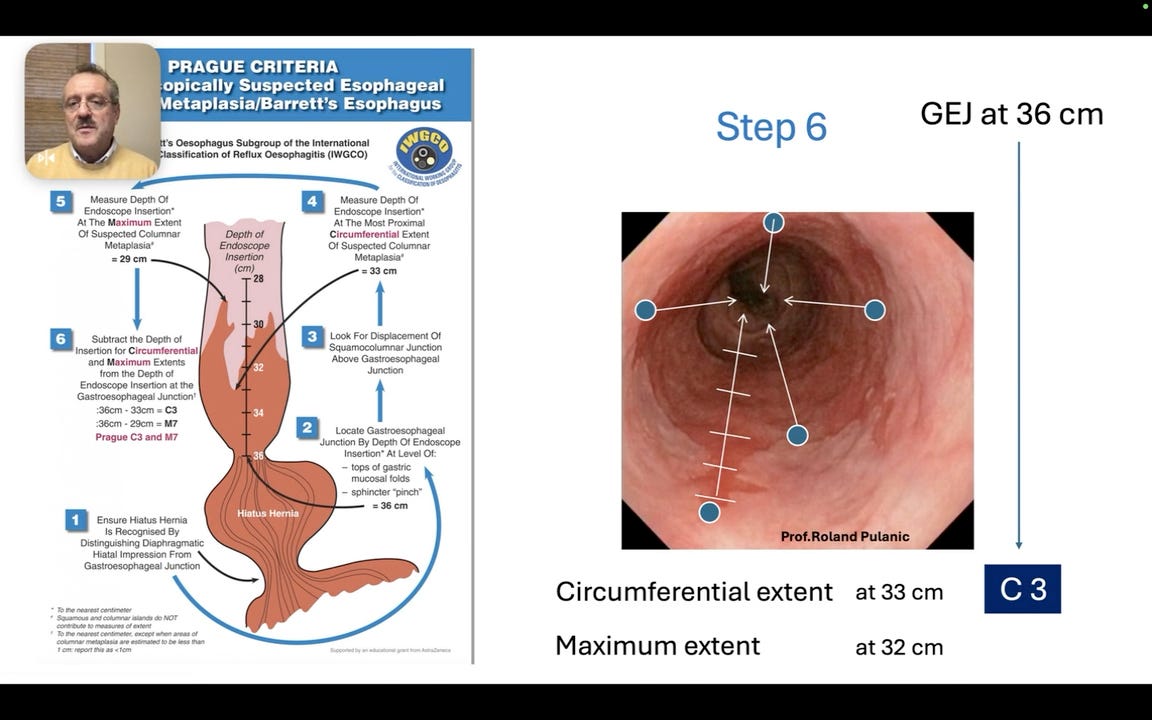
Step 5: Measuring the “M” (Maximal)
Continue pulling the endoscope back to find the absolute highest point of any Barrett’s tongue.
🖥 VISUAL ANALYSIS @ 10:47
The view shows a long finger-like projection of Barrett’s tissue extending upwards into the pale squamous mucosa.
Significance: The tip of this tongue represents the maximal extent of the disease.
The Calculation:
Locate GEJ (e.g., at 36 cm).
Locate tip of the longest tongue (e.g., at 32 cm).
Subtract the two: 36 - 32 = M4.
Result: This patient has C3M4 Barrett’s Esophagus.
Summary of the Prague Workflow
Find GEJ: Note the distance (e.g., 36 cm).
Find C-limit: Note the distance (e.g., 33 cm).
Find M-limit: Note the distance (e.g., 32 cm).
Math:
C = GEJ - C-limit
M = GEJ - M-limit