1 Mistake Endoscopists Make in Small Bowel Bleeding (And How to Avoid It)
A patient presents with obscure GI bleeding (OGIB). The initial EGD and colonoscopy are negative. The next step seems obvious: order a capsule endoscopy or schedule a deep enteroscopy. But what if that’s the wrong move?
In this expert walkthrough, Dr. Klaus Mönkemüller (Professor of Medicine) breaks down the most common mistakes in managing small bowel bleeding. He begins with a critical error that happens before a deep enteroscopy is ever considered—an error that, according to data, could be sending 30% of patients for unnecessary procedures.
This article analyzes Dr. Mönkemüller’s key insights, providing a clinical framework for avoiding this common pitfall.
Why Is Small Bowel Endoscopy So Challenging?
Before discussing mistakes, Dr. Mönkemüller provides context on why small bowel endoscopy is inherently difficult and high-risk.
Anatomy: The small bowel is long and convoluted.
Access: Simply reaching the lesion is significantly harder than in a standard EGD or colonoscopy.
Technique: The small bowel’s narrow lumen and very thin wall make it more challenging to maneuver and maintain an adequate resection position.
Risk: These factors (especially the thin wall) make the procedure more risky and prone to complications like bleeding and perforation.
Tools: The right accessories are not always available.
The First Mistake: Rushing to Deep Enteroscopy
The single biggest mistake, according to Dr. Mönkemüller, is performing a deep enteroscopy or capsule endoscopy too soon.
The reason this is a mistake is that in a significant number of cases, the bleeding source is not in the small bowel. It’s in a location that was missed by the initial EGD or colonoscopy.
To understand this, he first redefines the clinical problem.
Practice Point: Think “Mid-GIB,” Not “Small Bowel Bleeding”
Dr. Mönkemüller argues for using the term “mid-GI bleeding” (mid-GIB). He defines this as persisting or intermittent GI blood loss originating in the small bowel or an excluded stomach.
Why include the excluded stomach?
“Lots of patients have gastric bypass,” Dr. Mönkemüller explains, “and when you do an upper endoscopy or even a push enteroscopy, you will never reach the stomach... It’s in the mid-GI tract now.”
This diagnosis of mid-GIB is contingent on one key condition: a negative EGD and (ileo)-colonoscopy.
But what if that “negative” scope was a false negative?
The Evidence: 30% of Lesions Are Missed
Dr. Mönkemüller highlights data from a study he was involved in at the University of Magdeburg. The study looked at patients referred for double-balloon enteroscopy (DBE) to find the source of their obscure bleeding.
The findings were striking: “A lot of patients that were sent for us to undergo... DBE actually had lesions that were within the reach of EGD and ileocolonoscopy.”
A pie chart on screen (Lucia Fry et al. APT 2008) visualizes the findings:
54% of lesions were found in the small bowel.
16% had no lesions found.
30% had lesions outside the small bowel (i.e., within reach of standard EGD/colonoscopy).
This 30% represents the missed lesions. [PARAPHRASE] These initial scopes may have been performed in suboptimal conditions—for example, as an emergency, with significant blood in the stomach, or with poor colon preparation—all of which can lead to a missed lesion.
The “Must-Not-Miss” Lesions (That Are Frequently Missed)
So, what lesions are being missed 30% of the time? Dr. Mönkemüller provides a comprehensive list.
Frequently Missed Stomach Lesions
Cameron lesions
Dieulafoy lesions
Angiodysplasias
GAVE-syndrome (Gastric Antral Vascular Ectasia, or “watermelon stomach”)
Frequently Missed Colon Lesions
Angiodysplasias
Portal hypertensive colonopathy
Polyps or tumors
Other Missed “Upper GI” Causes
Hemosuccus pancreaticus
Hemobilia
Esophagitis
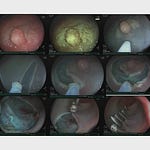
The presentation shows several powerful examples of these missed lesions:
GAVE: The top-left image shows the classic linear, erythematous streaks of watermelon stomach.
Cameron Lesions: The top-middle image reveals an ulcer found within a large hiatal hernia.
Duodenal Ulcer: The top-right image shows a duodenal ulcer, which the speaker notes was caused by radiation damage from SIRT therapy.
Stomach Angiodysplasia: A capsule endoscopy image clearly shows a stomach angiodysplasia that was missed on the initial EGD.
To see Dr. Mönkemüller’s analysis of the second major mistake in small bowel bleeding, his advice on negative capsule endoscopy, and his full list of 8 total mistakes to avoid, consider becoming a paid subscriber.
The First Take-Home Message: Repeat the Scopes
Based on this evidence, Dr. Mönkemüller’s first take-home message is clear and actionable.
First Take-Home Message
“EGD... and colonoscopy should be repeated before proceeding with capsule or deep enteroscopy.”
He emphasizes this may need to be done “two or three times.”
The rationale is simple: 30% of patients might have lesions that are within the reach of these standard scopes.Repeating the procedures, perhaps with a more experienced operator or in a non-emergent setting with a perfect prep, is a lower-risk, higher-yield next step than immediately advancing to a deep enteroscopy.
The Second Mistake (Teaser)
After solving the first mistake, Dr. Mönkemüller introduces the next common pitfall: “Relying too much on negative results of capsule endoscopy.”
He concludes this preview by noting he will discuss 8 total mistakes in his full lecture.
Poll & Discussion
How often do you repeat a “negative” EGD/colonoscopy in an OGIB workup before ordering a capsule?
🎁 Bonus Materials
1. Quick Reference Card: Missed Lesions in OGIB Workups
(Based on)
Before ordering a capsule/enteroscopy, repeat EGD/Colonoscopy and actively hunt for:
Stomach:
☐ Cameron Lesions (in hiatal hernia)
☐ Dieulafoy Lesions
☐ Angiodysplasias
☐ GAVE / Watermelon Stomach
Colon:
☐ Angiodysplasias
☐ Portal Hypertensive Colonopathy
☐ Polyps / Tumors
Other/Rare:
☐ Hemosuccus pancreaticus
☐ Hemobilia
☐ Aortoenteric Fistula
☐ Ulcerative Celiac Disease